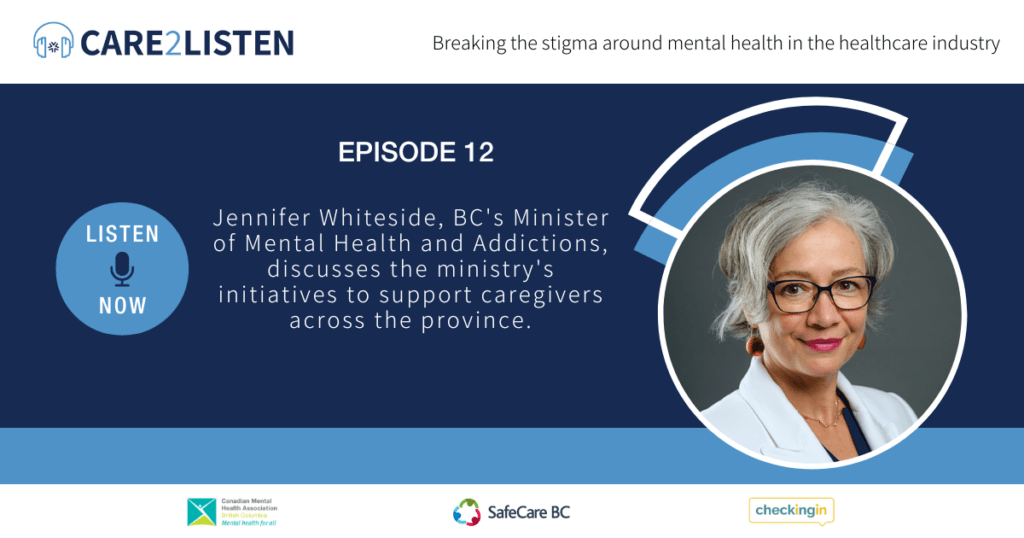
Episode 12 | Jennifer Whiteside
- October 23, 2023
Always, but particularly throughout the pandemic. I mean, we would not have survived in the way that we did as a society if we didn't have people showing up every day in hospitals, in long-term care [...], in, you know, social service agencies, in taking care of other people and making sure that all of the rest of us had access to the kind of care and support that we need.
Jennifer WhitesideMinister of Mental Health and Addictions
In this edition of the Care2Listen podcast, British Columbia’s Minister of Mental Health and Addictions, Jennifer Whiteside, provides further details about the Ministry’s efforts to assist caregivers around the province. This includes discussions on collaboration across ministries, the Overdose Public Health Emergency, and programs to address mental health issues in British Columbia.
Take this survey to let us know what topics you’re interested in.
If you want to share your story, please reach out to us at info@safecarebc.ca.
Resources
- Care to Speak | Care For Caregivers
- Phone Resources
- SafeCare BC: Your Mental Health Matters
- Home and community care pocketbook | Violence in the workplace – SafeCare BC
- Bounceback
This podcast is brought to you by:
Transcript
Sean Burke: Welcome back to another episode of the Care to Listen podcast. I’m your host, Sean Burke, and today we are recording at a new location, and I’d like to respectfully acknowledge the Songhees and Esquimalt peoples on whose territory we are conducting this podcast on. Joining me today is the Honourable Jennifer Whiteside.
The Minister of Mental Health and Addictions in British Columbia and elected MLA for New Westminster. Welcome to the show, Minister Whiteside.
Trigger Warning: this episode discusses topics that may be triggering for some viewers. Including addiction, suicide, and trauma.
Minister Whiteside: Hi, Sean. It’s a real pleasure to be here. Thanks for having me.
Sean Burke: So you’re somebody who has held significant roles, which include serving as the former Minister of Education and Child Care and working as the chief spokesperson and lead negotiator for the hospital. Employees union. So someone really qualified today when it comes to talking about what we’re here to talk about, and I’d just love to, before we jump into it, get to know a little bit about your backstory and what’s brought you into this role. So could you maybe share a little bit, you know, how you have come into this important role?
Minister Whiteside: Sure, Sean. Well, you know, I, I never really envisioned a political [00:01:00] career for myself. I was really very happy and had a really rewarding career working with health care workers which is what I’ve done for most of my adult life as part of being part of the labour movement.
And In 2015, I took on the role of the, essentially the CEO of the Hospital Employees Union. And as the Chief Spokesperson and Chief Negotiator when our government formed government in, in 2017, we had a really important round of bargaining in, in 2018, where we reestablish some, you know, fundamental health and safety protections for, for workers.
And what I’d say is that, you know, I, I think it was pretty evident heading into the pandemic that we had some real challenges around mental health issues in the workplace in particular, and really just, you know, I’m gonna cross kind of across, across all sectors. And then you know, in spring 2020, as we saw the pandemic sort of march across the globe and then have COVID 19 arrive in, in British Columbia.
We knew that that [00:02:00] was going to have a tremendous impact on every facet of life and particularly for, for healthcare workers who were really on the front lines of the pandemic. So for the first six months of the pandemic, I spent I, I spent that time working with government, with employers really Figuring out how to make sure that we supported the healthcare system, supported healthcare workers, and in particular, how we ensured that in long term care, where vulnerable seniors were the most directly impacted by by the COVID 19 pandemic, to make sure that those residents, those seniors, and the healthcare workers who were caring for them, were going to be as protected as possible.
Sean Burke: Yeah, and, and, you know, we saw new programs that were released through the Care for Caregivers program something that your ministry really took a lead and initiative on. This Care to Listen is an extension of that Care for Caregivers and it continues to grow. So, when you were looking at and I know that this was part of your predecessor who rolled [00:03:00] out these programs, but how has your ministry been able to continue the work that’s been done Since you took on this role?
Minister Whiteside: Yeah, well, it’s a funny sort of irony that my my, my, my friend and and neighbour and, and former, a colleague in the labour movement, Judy Darcy, who was the first Minister of Mental Health and Addictions and also an MLA for New Westminster I remember us getting a call from her one day saying, you know we have this idea about how we think we can provide supports for for healthcare workers during this, This really, this really challenging time.
And that was the care to speak. That was the, that was the peer to peer mental health support for, for workers. And that came on the heels of work that had been started to be introduced before the pandemic. The mobile workplace kind of emergence, urgent response team.
And so, you know, there had already been some work being done to try to figure out how to, how to, how to access, how to get to healthcare workers who can’t always, Who can’t always you know, go to [00:04:00] reach out or get to services the themselves. And so that really set an important groundwork and provided really important resources to, to, to healthcare workers.
And then of course, in the, in the, you know, I made the decision late in the year when we had an election in 2020 and Judy was retiring, I made the decision to run to, to run for the seat because I really believe that this is a time when. You know, we have really complex issues to take on in our, in our province, in our country, in our, you know, globally, as, as, as we’re experiencing now, and I think there’s never been a more important time to have a, have a government that really listens to working people and who will work with them to make their work safer, to make their workplaces safer better.
So that’s really something that we’re, that we’re very committed to and that, and it’s why we’ve really kept on with this work and continue to make these particular investments in building out the workplace hub as well so that we have, you know, digital resources available for people.
Not only healthcare workers, but really workers across all of the sectors that were, that were [00:05:00] really primarily hit by, hit by COVID.
Sean Burke: And, you know, hearing you talk about the challenges and the complexity and, you know, that being one of the passions and motivations for a lot of the work you’re doing, you know, oftentimes mental illness doesn’t. It’s not just one isolated issue.
You know, there’s many different ministries that are doing great work. And I’m curious about your specific platform. British Columbia was the first ministry of mental health and addictions to have such a ministry in Canada. And one of that primary focuses is to work across all ministries.
So when we’re talking about complex mental health issues, I’m curious how your team is working together with other ministries. to, to combat some of these challenges.
Minister Whiteside: Yeah, that’s a really important question, Sean, because this is kind of a unique ministry in that we don’t, we don’t have legislation that we’re, you know, kind of assigned to be responsible for.
You know, our, our, sort of our, our budget is really about trying to secure money for programs that other [00:06:00] ministries are going to, are, are going to, are going to deliver. It really is about leveraging. That work across Across Across the Health Ministry, the Education and Child Care Ministry, MCFD, other labor, you know, other, other ministries who are, who are actually developing the, implement, implementing the programs.
But, it’s really important to have a ministry that is really focused on What is an incredibly important and complex sort of set of issues that are, I mean, as you say, distinct from have often been thought of as quite distinct from physical health. So we have this sort of separation of our mental health from from, from our physical health.
But we really need to be working towards more of an integration. And that’s, that’s a really strong focus is to and I’m going to be talking a little bit about the work that we’re doing with our colleagues in the Ministry of Health, with our health authorities, to really integrate mental health and substance use into the work that they’re doing, so that, you know, if somebody go, you know, wherever they’re interacting [00:07:00] with primary care, if somebody shows up to their work.
you know, to their family practitioner or they go to the urgent care centre or wherever they’re accessing primary care, they can find a pathway. They can, they can get on a pathway to get the kind of support that they need because it’s not always as straightforward as it is with a broken arm, right. You know, you have a broken arm.
You go to the ER, they do an x-ray and get you cast, you know, cast you up so that you’re, and then maybe you’ll go do some rehab. But it’s much more. It can be much more complex with mental health and substance use issues.
Sean Burke: And it’s really interesting hearing you talk a little bit about the insight into how ministries work together.
In particular, I was picking up on the funding allocation and how the funding is allocated. And on some of the conversations we’ve had previously on this show, we’ve heard, you know, how come we just don’t have more support when it comes to you know, grieving a loss of having worked, had worked with a patient for so long.
And then, you know, you’re expected to, kind of, just put it behind you and move on to the next patient. I know [00:08:00] that there are some supports in place and we can touch on those in a minute, but I’m curious to take a step back from the actual specifics and learn and understand a bit more how your ministry is allocated funds is, is there a process in which your ministry needs to advocate for more funds or how does the funding work when it comes to your ministry and getting the resources that you need?
to deploy the resources that you’re hoping to deploy.
Minister Whiteside: Yeah, well, you know, part of it these are sort of some of the, the, the more the alchemy of how, how government works sort of behind the scenes. I mean, part of it, though, is that we have, I mean, of course, we have, you know, health authorities providing and, and, and delivering mental health and substance use services as part of their, sort of, their core mandate.
And that. Those additional resources that we’ve secured for particular programs when we know, for example, in 2021, we made a very significant investment specifically for mental health and substance use services. And we’ve seen the different ways in which health authorities have scaled up those services.
And in fact, just recently, [00:09:00] I, just last week, I announced some treatment beds that the Vancouver Island Health Authority is funding and that is a direct result of investments that we’ve made. And what’s important about the way that that program is going to work is that it is completely connected with Island Health.
So, the referral. For an individual who needs treatment will come through Island Health, it will come through the team of of, of of of doctors who are working with our community partners who have the, the beds in the, in the, in the, in the communities, and they’ll be making a decision about who gets matched to, to which bed.
Island Health will be monitoring the delivery of those, of, of, of that care, they’ll be evaluating it, monitoring it, so we’ll have a much more, sort of, seamless and much more eyes on. Approach to those, to those particular treatment beds. And that’s really what we’re trying to scale up across the whole province with health authorities, is having, again, those, those services really integrated to the work that health authorities are doing.
But another really [00:10:00] important area that we’re working on is child and youth mental health, which is terrifically important because we know how critical it is to be able to intervene upstream with youth. And so this is where our work with the Education and Child Care Ministry, my, my, my colleagues Minister Singh and Minister Lohr and Minister Deane and and Minister Children and Family Development is really important.
For example, in regard to the impact of the toxic drug crisis on youth, while we know that there is, we haven’t seen increases in substance use disorder when it comes to, to, to youth. We have certainly seen more, much more tragic and dramatic impacts as a result of the toxic drug crisis on youth, such that now toxic drug poisoning is the number one cause of death.
For, for youth, and that is, is a change that has evolved because of the, the poisoning of the, of the illicit drug supply. And so that really compels us to work collaboratively with education in terms of figuring out how, how do we talk to youth about [00:11:00] drugs, what and about the risks of substance use.
in the context of you know, of the, the really you know, ter terrible and, and volatile toxic drugs, drug poisoning crisis that, that we’re in right now. How do we work with MCFD when we know that 75 percent of the youth who die from toxic drug poisoning are involved with MCFD?
So those are ways in which we’re all working together to to find answers, to, to find, to find some solutions to those, to, to, to that problem. that part of the crisis.
Sean Burke: And no doubt an extremely difficult and complex situation, problem crisis. And, you know, unfortunately we just surpassed 13, 000 deaths since this has been declared a public health emergency.
So from your perspective when it comes to that work, that collaboration that’s really being done, is there a specific Not solution per se, but strategy that’s really being focused on when it comes to addressing some of the challenges that we’re [00:12:00] seeing and the rate of the increase of deaths that we’re seeing.
Minister Whiteside: Yeah, well, you know, I, I would say that first and foremost, it’s important to understand the nature of the emergency that we’re in. It’s not a public health emergency in the same way that we had sort of the COVID 19 public health emergency where it was a virus. We knew how to treat it. And we had to implement very dramatic public health measures to keep people safe until we could until we got the protection of vaccines.
And you could really see sort of a beginning and a middle and a, and a Of the vaccines were of course not, A transformation into something different for that particular health emergency. The toxic drug emergency is just a terrifically wicked problem because in part, you know, it’s driven by a toxic drug supply, which was made so much worse by our [00:13:00] experience through COVID.
It is a challenge in terms of all of the pillars that we bring to bear on, on this problem and have historically from, you know, enforcement to prevention to treatment and to, and, and to recovery. All of those. It’s, you know all of those, those pillars are really critically important, but really challenging for, you know, law enforcement.
You know, we’re doing everything we can to separate, try to separate people from the toxic drug supply trying to look at the upstream you know, issues and, and, and prevention, particularly around, around children and youth. But you know, that it has you know, this crisis has so many different antecedents, right?
I mean, as many people who experience addiction, like there are, there are So many pathways into that, into addiction, and there have to be, you know, all of, as many pathways out of it. And so building a system of care for people that is, that provides them with the, the right support, the right care, at the right time, sort of [00:14:00] when they need it for a disease that is a chronic and relapsing disease is is, is, is really complex, you know.
We You know, we, we, we had a, we had a sort of a, a landscape in this part of our healthcare system that was really underfunded, deregulated, and privatized for much of the, the, the 2000s, up until we, up until we formed government, and so we are trying to knit together all of those threads to form a real, a real net for people, and this is what I keep in my, this is what I think about every day, is that we really have to have a net for people.
And we have to try to make sure that their, that, that the way in which they can access care is as seamless as possible. anD so that’s what, that’s really what we’re working on is, is trying to ensure that people get access to the care that they need in, in a, in a seamless way as, as possible.
Sean Burke: It sounds very much like meeting people where they’re at, and, you know, it can be really difficult because people are at all different [00:15:00] stages. aNd in particular, in the recovery, like you said, the, you know, sometimes there’s steps forwards, and then, you know, someone might relapse, or, you know, go through some of the challenges, and they know the impact not only stays with the individual who’s experiencing those challenges, but also to, to their wider supports.
So, I, I’m curious as we sort of jump back into, you know, what the ministry and what the government of BC has done when it comes to stop overdose BC there’s a lot of work that’s being done in the province. And in particular, I’m thinking about the recent steps that were taken on January 31st, 2023, where BC decriminalized the use of certain drugs.
And I’m curious from your perspective what sort of impact or what sort of changes have you seen by, by taking those steps and those actions?
Minister Whiteside: Well, it’s still, I, I, I’d say pretty early days, even though we’re almost 10 to 9 months into it now. But I, I think we, you know, we anticipated that it would be a [00:16:00] slow process of having that change work through, work its way through the system.
And the, you know, the primary objective of decriminalization, which really had been called for by law enforcement it had been called for by public health, by front line physicians and, you know, nurses who, who take care of people, who provide care for people who are struggling with with addictions.
We had a wide range of partners really calling for changing up that relationship between what happens when people who are carrying small amounts of illicit drugs for personal use, and it’s really clear that it’s It’s, it’s personal use. They’re not, they’re not, they’re not trafficking.
Changing that up so that we don’t have police officers kind of engaging in a kind of criminal, through a criminal justice lens with those individuals. We use any interaction that’s going to happen between law enforcement and those individuals as an opportunity to, again, connect them to care. And through that process.
this work to, to, again, push on [00:17:00] taking, taking away some of the stigma and fear that’s associated with drug use because we don’t We don’t want people to be using alone because it is so risky these days It is so risky given the toxicity the drug supply for people to be using alone We want people to feel like they can reach out And, I just, you know, I will never forget talking with Catherine Botchford, whose husband was a journalist and, and who died of a of a, of an overdose in their basement.
And she didn’t know, she didn’t know that he was using drugs. You know, I didn’t know whether he used them, you know, a handful of times or frequently. And that, you know, the dramatic impact of that on, on her, I mean, life changing for her and, and, and her family. And the questions around, you know, if you’ve got a loved one who has died from toxic drug poisoning, you’re always going to be wondering, is there something that could have been done differently?
Could I have reached out in a different way? Should I have done, should I have done something different? And we don’t want any family to feel that any family to be, to be in that position. So working [00:18:00] to, you know, remove the fear and, and stigma associated with it so people feel like they can reach out, because again, you know what to do if you’ve got a broken arm.
You don’t necessarily know what to do if you’re if you, if you have an addiction issue but you might not even really know that you have an addiction issue. You just may be aware that you have a problem or you might be concerned about some of your substance use. People need to be able to, need to be able to reach out.
Sean Burke: And so back to that healthcare worker who’s You know, feeling overwhelmed or maybe, you know, challenged with some of the unique pressures that they might be facing. If they are using substances to cope with some of those challenges or issues, what would you say to them?
Minister Whiteside: Well, you know, first of all, I just want to say that, you know, I mean health care workers have gone so above and beyond and done such incredibly just extraordinary work.
Always, but particularly throughout the pandemic. I mean, we would not have survived in the way that we did as a society if we didn’t [00:19:00] have people showing up every day in hospitals, in long term care facilities, in, you know, social service agencies, in taking care of other people and making sure that all of the rest of us had access to the kind of care and support that we need.
And, you know, we, we can never forget the incredible contribution that healthcare workers made to getting us all through an unimaginable time for us. I mean, really kind of a collective existential crisis. Something we have not experienced, any of us, in our lifetimes. And that was You know, for, for, for my, for, for my, you know, my mother, who was, who, who died last year, but was in her early 90s and in long term care, and got, got COVID, and got, got through, through COVID.
You know, I mean, she, she remembered although she didn’t live through it, she remembered, you know, the Spanish flu in, you know, after, after the First World War. But, you know, that something, that this was not something that any of us had lived through. And What, what health care workers did was, was remarkable, and I understand that the [00:20:00] pressures on health care workers today are are, are, are extraordinary.
I mean, we are, we talk about being sort of, you know, out of the pandemic. I mean, we’re certainly out of the acute phase of the pandemic, but we know that COVID continues to have, you know, a significant impact on our healthcare system. You know, we’re, we’re in a world now where, where we want people to stay home when they’re sick because we don’t want to risk transmission of COVID 19 and other respiratory illnesses, but COVID 19 can still be very, you know, serious for vulnerable populations.
So we’re in kind of a different a different, a different world now and it you know, that compounded with the, you know, an interesting fact that we don’t necessarily think of in connection with this, but, you know, over 200, 000 people moved to British Columbia in the last two years. We’ve seen rates of immigration to British Columbia that we have not seen in decades, maybe ever.
And that means that all of those folks need access to health care, to doctors, to you know, education, to all of our, you know, all of our, our [00:21:00] services. And our, we’re working hard to try to catch up our, our health human resources with that, with that picture. But it’s hard these days. In, in, in health care.
So I understand that health care workers are going through a lot. And I just would, would strongly encourage health care workers to, you know, if there’s somebody that they can reach out to talk to in their family, you know, in their workplace, in their union to, to, to do that.
Sean Burke: Absolutely. And, you know, we’ll make sure that in the show notes we put some of those resources that are available. So be sure to check that out as well. Jumping into a little bit more of You know, the ministry’s Pathway to Hope report, or the update that was recently provided. I’m also going to bring in the In Plain Sight report that was also performed.
I’m curious to hear, you know, in that Pathway to Hope report, one of those key pillars for the ministry’s strategy. Was to, to really have strong Indigenous led solutions. And so I’m curious if you could touch on what your ministry is [00:22:00] doing when it comes to supporting more specific Indigenous led solutions.
Minister Whiteside: Yeah, thanks. That’s a really important question. We know that First Nations and Indigenous people are disproportionately impacted by mental health issues and by the toxic drug crisis as well. Indigenous people are four times more likely to die from toxic drug poisoning. Indigenous women, eleven times more likely to die from toxic drug poisoning.
So, you know, there are many many reasons for that, having to do with colonialism, racism, you know, intergenerational trauma, many things that, again, are, are specific, you know, particular issues for, for, for those populations. And, and so we, we understand that it is, It’s critically important for Indigenous people to lead their own, their own solutions and for us to support that.
And, you know, if there’s anything that I really learned on the, in the first the first couple of months on the job in this file is that community really saves lives, [00:23:00] but culture really saves lives. Culture really saves lives. And so ensuring that we have culturally you know, appropriate culturally led services in place is, is really key.
And, and so we’ve been working directly with nations. We work through the First Nations Health Authority. And we have some programs that are funded and developed in conjunction with the federal government to provide treatment services. for Indigenous people for First Nations.
And in this past budget we allocated 171 million for Indigenous led treatment and recovery programs that will, you know, will, will look differently across the province. But working really closely with nations like where that, where, where that goes and how, what kinds of services get scaled up with that.
Sean Burke: And really what I loved hearing about that, that response too is that it’s a, it’s not a one size fits all, and it’s a one size fits one nation approach, and being able to have that self determination and those [00:24:00] communities lead and bring forward some of their own solutions is such a really strong way for communities to, to lift up and support their community members.
So, definitely applaud your ministry in that regard. When it comes to a little bit more of a long term vision, and I think sometimes this might be a little bit of criticism that different governments get from time to time, it’s a little bit more short sighted. What is your ministry doing from a long term vision perspective?
Yes, there’s the importance of, you know, dealing right now with the crisis we are seeing but what about the long term solution. This isn’t going to be a problem that is fixed overnight.
I’m curious what your sort of forward thinking plan is with your team.
Minister Whiteside: Yeah, I mean, and it is, again, again, for me, it really gets back to how we transform our healthcare system, to also be always thinking of health and mental health and substance use as part of, part of the, part of health as, as well.
[00:25:00] And so we, sort of, laid out our vision in Pathway to Hope, our 10 year strategy on mental health and substance use care. And we’re sort of, you know, working through, you know, made lots of progress on particularly the, the preventative side and the upstream services in, in regards to children and youth, and clearly more work to do there.
You know, we’ve done things like ensure that we have community, low barrier community counseling. Resources available for people, again, as a sort of an upstream preventative Kind of access to lower barrier services. And then again, it’s working with health authorities to really integrate the care and treatment.
So for example, St. Paul’s right now is working on a sort of a seamless model where. an individual would come into their, come into the hospital through, through ER, through, through their Rapid Access addiction clinic maybe. And they would get referred to a stabilization, a detox and stabilization bed they’d be, they’d be cared for while they’re in withdrawal management and then they transition right into [00:26:00] treatment.
And then from treatment they transition to an aftercare program and it would be, sort of seamless. and sort of met all, all, all under the auspices of, of, of the Health Authority. And I think it’s because you know we are always going to work with community partners. We have very many excellent community partners who deliver services in, in this space, and, you know, making sure that we are, that we have the right the right sort of approach to When when the health authority is delivering services, when they’re working with community partners to deliver services, that is that, that’s also a big part of what we’re doing right now.
Because we really have to look at them, we really have to be building up the evidence. We have to understand what kind of approach to treatment works in certain situations. We know that bed based treatment works for some people in some circumstances. We also know that outpatient treatment can work.
People can be, some people can be supported to detox, for example, successfully at home. They can be, they can be in a treatment program. But, but be, but be supported to do that from home. [00:27:00] So, you know, again, kind of meeting people where they’re at and having the right kind of service for, for what they need.
That, that is that, that is work that we’re, that, that we’re, that we’re engaged in. And really having things like like our early psychosis intervention program, which is which we invested over 58 million a couple of years ago in scaling up and investing in the, the, the, the health care providers that we need in order to make sure that that, that youth, when they are interacting with the health care system if they need support for for mental health issues that they have access to that, to that dedicated program.
So there again is, you know, it is about working with health authorities and working sort of, provincial services and regional services. So that just as, just as if, you know, if you’ve got a broken arm and you know you can get care at the hospital. You know, if you’re having a mental health issue, you know that you can, that it, that you can go and get, get the help you need at the hospital.
And you may not need hospital based help. You might need some other kind of help, but we’re going to help you [00:28:00] figure out what’s going on and then trans, get you transitioned to the care that’s right for you. the particular care, care that you need. Absolutely.
Sean Burke: Well, we have certainly covered a lot today.
And I know there’s tons more questions that I’d love to get to, but I really feel like today we’ve been able to capture a wide range of topics and to also just re emphasize that if you are a healthcare professional and you are struggling or you do need supports there, There are platforms, there are services that are available for you and again, we’ll make sure that those are available in the show notes.
Very briefly as we sign off here, I’m curious if there’s anything we haven’t covered today you know, or any messages that you’d like to offer to those healthcare practitioners listening today.
Minister Whiteside: Well, you know, again, I just, I want to come back to the extraordinary work that folks are doing on the front lines.
You know, I’ve had a chance to tour the province over the last few months, and I’ve seen you know, I’ve seen peer outreach workers do incredible, incredible work. People who were [00:29:00] homeless and lived on the street for a long time, who found their path. Found, found a wellness journey that worked for them and are now employed in the, in the, by the Interior Health Authority doing outreach, supporting people who are kind of where they were 20 years ago.
And it is incredibly moving to see the commitment and the dedication that they bring. to that kind of work. I know there are so many workers across our supportive housing sector, for example, who are working with people who have mental health and substance use issues doing incredible incredible work supporting them.
And I, I think a lot about the the, the street out, outreach workers who, you know, load up backpacks and with, you know, wound care supplies and food and granola bars and insure and and, and, and go out and meet people where they’re at and provide care for them. And I have been so moved by the incredible compassion of really, again, meeting people where they’re at and treating people with such, like, with the utmost of dignity.
When [00:30:00] they’re sometimes at their worst, sometimes having their worst moment. But always being able to find the human value and the dignity in, in everyone. And I think about that every day. I’ve had, you know, particular experiences that I’ve been part of where I have been really, really impacted by just the incredible dignity and sensitivity and compassion that healthcare workers are bringing to their work.
But I also know that it takes a toll. You, you don’t do that work without, without it taking a toll on, on, on, on you. And I really really want health care workers to know that we’ve got their back. You know, we brought in a presumption, presumptive coverage for for for certain occupations. in, in, in British Columbia to recognize that there are some jobs that just come with a higher rate of mental health distress than, than others and that we need to make sure that the pathway for, you know, through WorkSafe is, is easier for, for, for people so, you know, we have, we have we have the, the [00:31:00] resources that we, that we do that, that we provide in conjunction with the Canadian Mental Health Association of B.
C. which I, as a partnership I’m very, I’m always deeply grateful for. So there are resources there are resources out there and I really, Really, really I just want people to take care of themselves because I know it’s tough
Sean Burke: out there. Absolutely. Well, thank you very much for taking the time today, Minister Whiteside.
We really deeply value your insight, your time, your ministries, all the hard work that is going into, you know, trying to make BC a great place to live. And when people are struggling to recognize that, you know, that, that happens and, you know, it’s okay to put your hand up and to, to get that support, get that help that you need because it impacts us all whether you’re the person struggling with mental illness or you’re the person that’s supporting.
So we, yeah, really deeply value your time, your insight and all the hard work that your ministry is doing. So thank you very much for coming on the show
Minister Whiteside: today. Thank you so much for the conversation, Sean, and shout out to all the health care workers out there.
